The University of Benin Teaching Hospital (UBTH) stands as a cornerstone of healthcare delivery and medical training, epitomizing medical excellence in Nigeria. Established in response to a Government Edict in 1972, UBTH has long been a pioneer in healthcare delivery and medical education within Nigeria. Over the years, it has evolved into a leading teaching hospital and tertiary referral center, not only meeting the healthcare needs of Edo State but also attracting patients from neighboring states and beyond. Under the leadership of CMO Professor Darlington Obaseki and the hospital’s unwavering commitment to providing top-tier medical care, coupled with its esteemed reputation for excellence, UBTH is ideally positioned to spearhead advancements in specialized medical services such as urology.
Department of Urology at UBTH
The Urology Unit at the University of Benin Teaching Hospital (UBTH) stands as a testament to a legacy of excellence. Established alongside the hospital’s inception by a Government Edict in 1972, the Urology Unit commenced its journey of service and education in February 1973. For over five decades, it has remained a steadfast beacon of specialized medical care and a stronghold of medical education in the region. The establishment of the Unit was a visionary response to the increasing prevalence of urological disorders, underscoring the hospital’s dedication to addressing complex healthcare challenges.
UBTH’s influence transcends its geographical boundaries, extending not only across Edo State but also encompassing neighboring regions such as Delta, Ondo, and Kogi States. Moreover, its strategic location along the River Niger positions it as a vital referral center for a wide expanse of the country. Patients from distant states seek out the specialized care offered by UBTH, reaffirming its role as a tertiary referral hub for urological conditions. The Urology Unit, alongside other specialized units, serves as a hub of expertise, attracting patients from various corners of the nation.
Current Services:
The department currently comprises five consultants, with Professor Sam Osaghae serving as the head of the department. The Urology unit boasts approximately 20 inpatient beds and one operating theater. Presently, the department’s expertise lies in endoscopic urology, including TURPs, TURBT, Ureteroscopy, ESWL, and open renal surgery. The department’s theater setup, outpatient clinics, diagnostic urology, inpatient care, audit, and research endeavors are all meticulously organized and efficiently run.
The department plays a pivotal role in shaping the medical school curriculum and nurturing the next generation of medical professionals. The Urology Unit has served as a crucible of training for Urological residents and fellows, molding them into skilled urologists. Many of these trainees have gone on to become distinguished Fellows of the West African College of Surgeons (WACS) and the National Post-graduate Medical College of Nigeria, underscoring the Unit’s commitment to producing highly qualified medical professionals who significantly contribute to the field. The Unit’s training approach emphasizes a blend of theoretical knowledge, clinical exposure, and surgical proficiency, fostering the development of well-rounded urologists.
1st Laparoscopic Urology Masterclass 11-15th September 2023

Following significant progress in establishing laparoscopic urology at Hospital General Idrissa Pouye Dakar, Senegal, via their links, the UBTH Department of Urology approached us for support in establishing similar laparoscopic services in their department.
The objective was to establish a recurring structured workshop every 6-12 months, with the inaugural workshop conducted from 11-15th September 2023.
Pre-Workshop Preparations:
Thorough pre-workshop planning was undertaken to ensure the success of the five-day workshop. This included procuring necessary equipment for safe operation. Some equipment was purchased, such as laparoscopic scissors, right angles, suction, hemlock applicators and clips, and simulation tools, while a significant portion was acquired through donations. This included energy dissection devices, laparoscopic ports, hand gel-ports, and grasping forceps.
Cases for the workshop were discussed via WhatsApp and Zoom meetings prior to the start, to select the most suitable candidates. A scientific program was scheduled to allocate time for lectures, simulations, and live hands-on training during the week.
Workshop Experience:
On the first day of the workshop, the first half of the morning was dedicated to meeting hospital senior management, who exhibited great engagement and proactivity. We were given a tour of the hospital, during which the working ethos and future goals of UBTH were highlighted. This provided us with a strong sense of commitment from the host team to advance the project further.
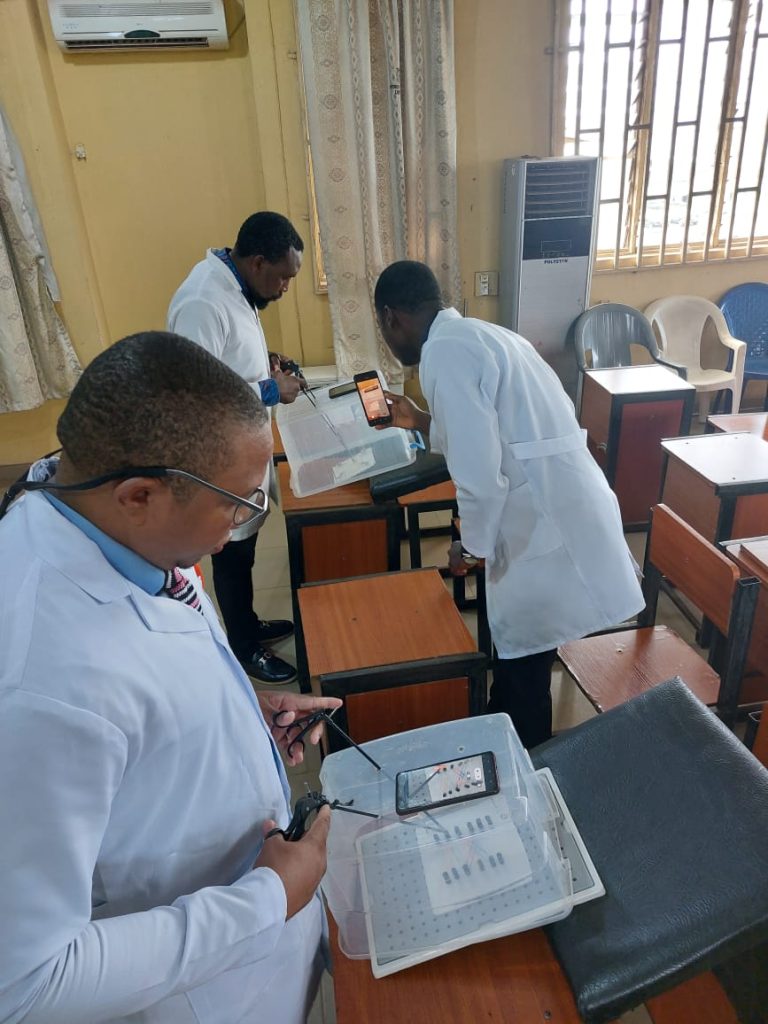
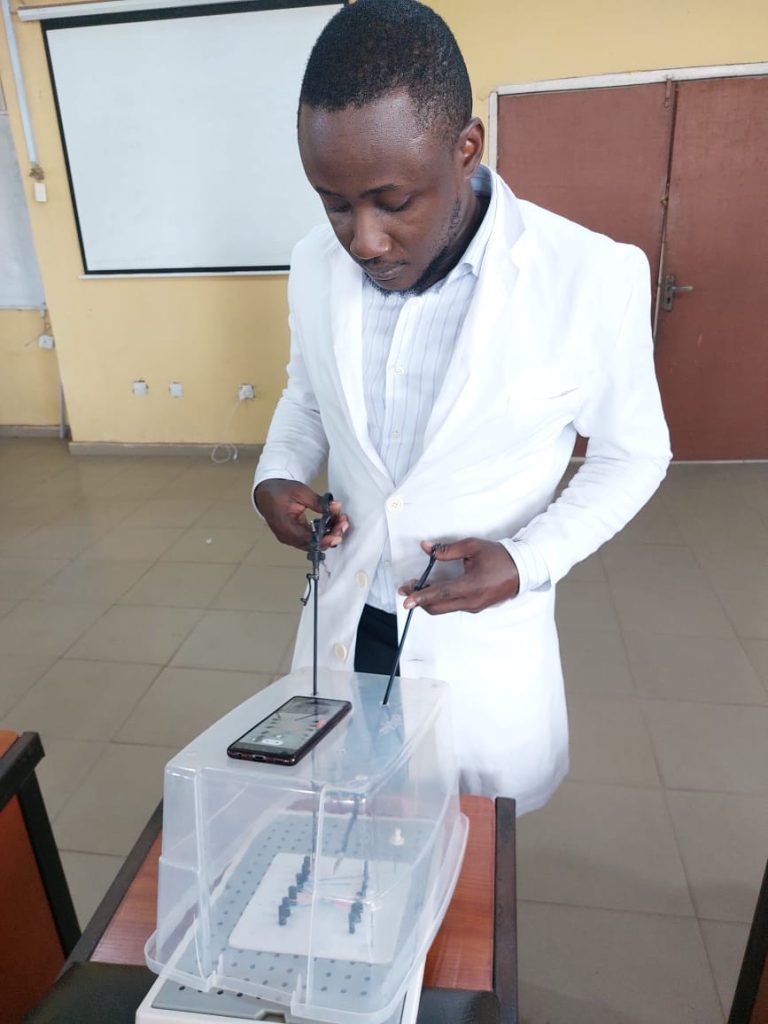
A typical day during the workshop week commenced with a ward round, followed by an hour of lectures on laparoscopy. On the first morning, we introduced residents to simulation exercises, which they continued throughout the week, alongside attendance in operating theaters to observe live surgeries.
From mid-morning until late evenings, both faculty members, Zeeshan Aslam and Ali Thwaini, provided live hands-on training to consultant colleagues. A total of seven laparoscopic procedures were performed, including a case of decortication of a renal cyst, three nephrectomies, and three pyeloplasties. The concept of training the trainer was adhered to among the host team, with two senior consultants trained to work together.
The renal cyst case served as a starting point to provide exposure to basic skills such as patient positioning, port placement, bowel mobilization, and use of common instruments and energy devices. We gradually progressed to laparoscopic nephrectomy to refine dissection skills, alongside safe handling of the renal hilum. The host team performed the majority of these procedures under supervision, with some assistance in demonstrating hilar dissection as required.
The three cases of pyeloplasties provided further opportunities to refine these skills.
However, due to the advanced level of skills required for reconstruction, laparoscopic suturing was performed by the faculty. During the initial laparoscopic workshop, we did not anticipate the host team to demonstrate proficiency in suturing.
In comparison to my previous laparoscopic workshops in Senegal and Pakistan, one of the modifications we introduced is the use of gel-ports for hand-assistance during critical parts of the procedure, such as renal hilum dissection. This addition provides the team with additional confidence and security while performing procedures, hopefully resulting in a more accelerated learning curve.
All seven cases were completed laparoscopically without any complications. By the time we performed the seventh procedure, the host team had demonstrated significant improvement in their skills and confidence levels. All seven patients experienced a good recovery without immediate post-operative complications and had much shorter hospital stays, significantly lower post-operative pain, and early mobilization compared to open procedures. Unfortunately, one case of pyeloplasty was readmitted with sepsis and was found to have a post-operative collection requiring drainage.
Positives from the workshop:
The host surgeons demonstrated the ability to learn and retain taught skills, showcasing safe operating throughout. During the debrief on the last day, both my co-faculty and I felt that the team had reached the desired level of competency to start independent operations with simple cases such as decortication of renal cysts and pyelolithotomy for large renal stones.
The anesthetic team displayed brilliant knowledge and skills in running laparoscopic skills, providing invaluable support to the surgical team, which is of paramount importance.
The residents demonstrated admirable passion and commitment to laparoscopy, which is crucial for the future of laparoscopy in the region.
The theatre scrub team exhibited all the necessary knowledge to run laparoscopy lists and to look after the instruments as we would have liked, thus prolonging the lifespan of the equipment.
Future goals:
Our experience of the first workshop exceeded our expectations. A young host team demonstrated enormous potential and commitment. This is evident by the fact that the host team has started independent procedures, including pyelolithotomies and nephrectomies. Moving forward, we aim to acquire more equipment for the department. We plan to conduct at least one more workshop during 2024 focused on nephrectomies and pyeloplasties, which I am hopeful will provide them with adequate experience to gain proficiency.